by Agnies Calkoen
NHS England’s Chief Medical Officer, Professor Dame Sally Davies, states antibiotic resistance kills 5,000 people in the UK each year. Yet at least 12,000 people in the UK are likely dying each year from drug-resistant sepsis (blood poisoning) alone, according to Dr Ron Daniels, Chief Executive of the UK Sepsis Trust.
Although antibiotics have been the gold standard for treating bacterial infections since the advent of penicillin around 90 years ago, our misuse of these drugs is gradually rendering them useless. Not finishing the course, prescribing them when they’re not needed and using them with livestock are all contributing factors.
So what are these superbugs and how can we protect ourselves and our communities?
Agnies is a Sensory Herbalist who is also a GP working within the NHS we asked her to write about MRSA, the so-called superbug.
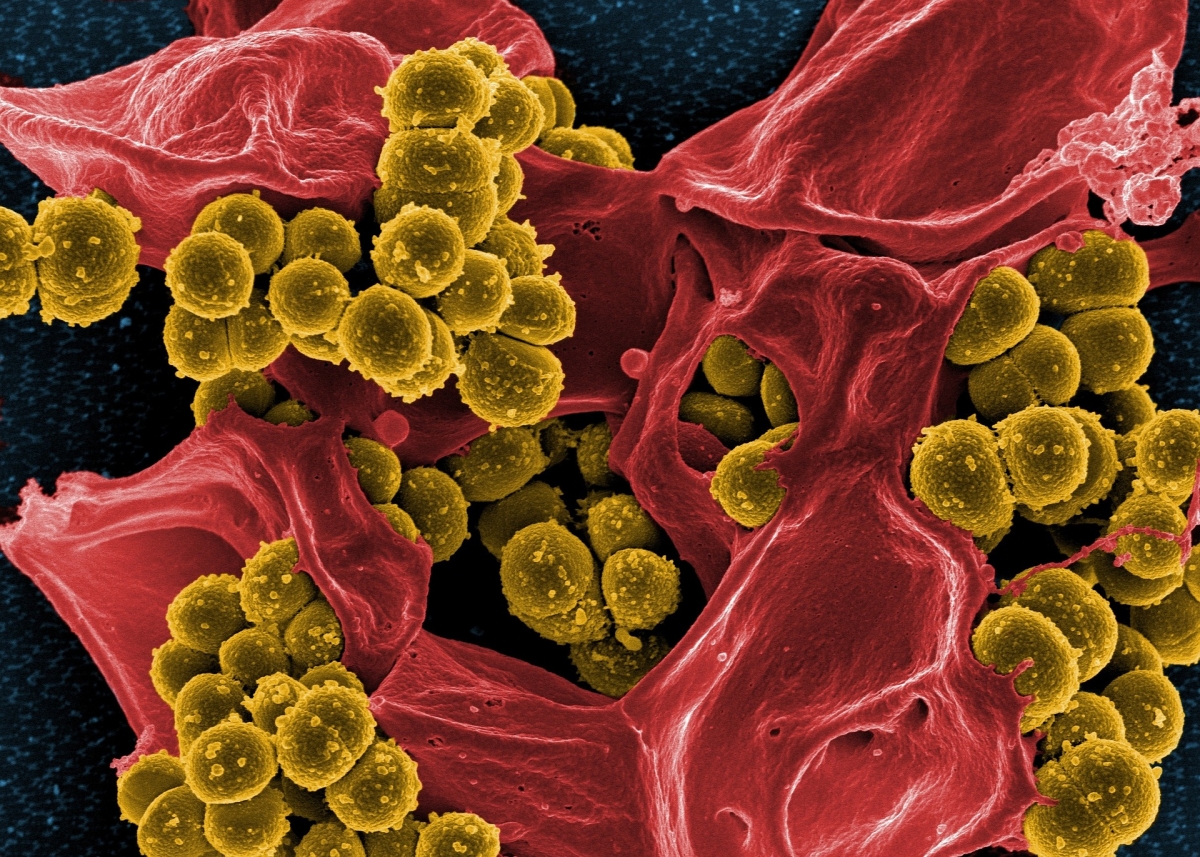
MRSA (Methicillin-Resistant Staphylococcus Aureus) is a strain of a bacteria, an organism called Staphylococcus aureus. This strain is resistant to some of the most common antibiotics, which is causing great concern within the medical establishment.
Staphylococcus aureus is actually very common. Most of us carry it on our skin, particularly the nose, skin folds, hairline, perineum (the bit between your front and back passage) and navel. It commonly survives in these areas without causing infection. This is what is known as ‘colonisation’. But if the bacteria invades on a deeper level and multiplies, it soon becomes an infection.
Signs of infection usually are redness, swelling and pain. The immune system works hard to contain the infection by raising the body temperature (fever) rendering the bacteria ineffective as it cannot survive and thrive at those temperatures. Staph aureus normally responds well to variations of Penicillin, one of the first known antibiotics.
The term MRSA was first coined in the ’60s. Initially MRSA was seen mainly in hospital environments but unfortunately since the ‘90s it started to be seen more often out in the community. Within the NHS the focus is on preventative measures; washing hands has become almost a compulsive habit. ‘Barrier nursing’ is implemented, when there are known carriers of infection, meaning health care professionals, will wear disposable gloves, an apron and often a face mask when delivering care.
The big issues are with the very young, the sick, the immunocompromised, people undergoing chemotherapy, or in the hospital / care home environment which generally has lots of organisms around that can easily be passed on from one person to next. All sorts of bugs can opportunistically cause infections.
Little is being spent on research and development of new antibiotics because drug companies see small returns on their investments.
For a long time, medieval medicine which is actually herbal medicine has been dismissed as irrelevant. This time period is popularly referred to as the “Dark Ages,” which erroneously suggests that it was unenlightened by science or reason. However, some scientists are now looking back to history for clues to inform the search for new antibiotics, suggesting that herbs may actually have the answers to this worldwide health crisis!