Danny O’Rawe is a well-known herbalist, working in the field of natural medicine since 1986. His diverse training has since taken him from a Diploma in Herbal Medicine to the shamanic traditions of the Amazon rainforests to a Master of Science degree in Herbal Medicine.
He is an honorary Fellow and former president of the Irish Register of Herbalists, Ireland’s leading association for professional herbalists. He is the founder of Plant Healer Federation and a founder of the annual Herb Feast festival in Ireland. He is a Royal Horticultural Society trained grower with over 25 years’ experience. He is a researcher, activist, author and consultant clinician with a busy multidisciplinary practice in Belfast.
Introducing Danny:
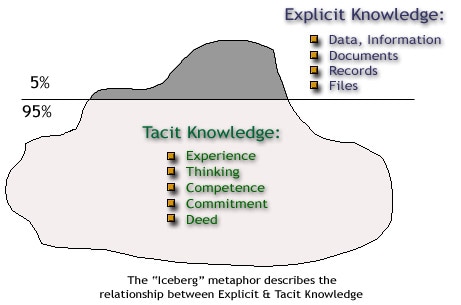
Danny O’Rawe is founder of the Plant Healer Federation, which creates a forum for exploring the ways in which plant medicine could be integrated into mainstream medical options. He talks about acceptance of ‘tacit’ knowledge…that is something that can only be known from within, from years of observations and expertise. Tacit knowledge is something embraced on our own Sensory Herb Apprenticeship.
Danny’s takes on the politics and possibilities of medicine are both challenging and hopeful, spiritual and scientific. This is a detailed and thought provoking article.
“Trees are poems the earth writes upon the sky.
We fell them down and turn them into paper,
That we may record our emptiness”
(Kahlil)
“We can Know more than we can tell”
(Polanyi)
The Plant Healer Federation was set up in the wake of the World Health Organisation (WHO) Traditional Medicine Strategy 2014-2023 published in 2014. The document presents the case for the integration of traditional medicine into a modern health care system. The reasons for this are that modern Biomedicine has become so expensive and unwieldy that it is impossible to bring doctors and proper hospital/clinical facilities to all corners of the globe.
In terms of global healthcare sustainability therefore, WHO feels it is necessary and urgent to develop local and traditional forms of medicine and explore ways and means of integrating them into a modern healthcare system. Traditional forms of medicine are largely plant based forms of herbal medicine, which stretch back many centuries.
“Many countries now recognise the need to develop a cohesive and integrative approach to health care that allows governments, health care practitioners and, most importantly, those who use health care services, to access Traditional and Complementary Medicine (T&CM) in a safe, respectful, cost-efficient and effective manner. A global strategy to foster its appropriate integration, regulation and supervision will be useful to countries wishing to develop a proactive policy towards this important – and often vibrant and expanding – part of health care” (WHO, 2014).
Initially I thought that this was good news. At last, there was some recognition in the corridors of Western medical hegemony that traditional medicine has something to offer. However, within the WHO document there is the caveat of evidence-based medicine (EBM), and so although traditional medicines could be made part of the integrated system WHO propose, they have to prove themselves first through systematic research.
What this means is that even though traditional practices of medicine are as old as civilisation, and their remedies and practices are tried and true, they still need to meet with the criteria of EBM. This means running expensive double-blinded randomised controlled trials to prove the safety, effectiveness and efficaciousness of herbs. There are multiple problems with this approach, which goes to the heart of the current medical hegemony.
Although the document seems aimed at Developing Nations in particular, where medical infrastructure is most lacking, the spirit of the letter applies internationally. Traditional forms of herbal medicine have been practiced in the West since the earliest times. Western Herbal Medicine (WHM) must therefore be considered a traditional medicine, and yet there have been no conversations between WHO member states and the representatives of WHM. If there is an urgent need to integrate traditional medicine, then surely it begins with conversations with those practitioners who hold traditional knowledge. I have spoken to many groups about this, and none of them have received any communication in this regard.
Despite this, part of the emphasis of the WHO strategy is to encourage what they call “rational use — promote therapeutically sound use of appropriate TM by practitioners and consumers” (WHO, 2014). WHO acknowledges there will be difficulty in this process and they have outlined policies to help member states address any issues:
1. build the knowledge base that will allow T&CM to be managed actively through appropriate national policies that understand and recognise the role and potential of T&CM.
2. strengthen the quality assurance, safety, proper use and effectiveness of T&CM by regulating products, practices and practitioners through T&CM education and training, skills development, services and therapies.
3. promote universal health coverage by integrating T&CM services into health service delivery and self-health care by capitalising on their potential contribution to improve health services and health outcomes, and by ensuring users are able to make informed choices about self-health care” (WHO, 2014).
Let us consider these points.
In Point 1, building a knowledge base begins with the acceptance that those with traditional knowledge hold intellectual property. This property must be safeguarded against exploitation such as the theft of plant knowledge for the development of novel compounds by the Pharmaceutical Industry. WHO need to clarify what is meant by “appropriate national policies” which suggests a top-down approach and does not seem to recognise the primacy of the herbalist or their tradition?
In Point 2 the position is that Traditional and Complementary medicine (T&CM) must meet with quality assurance, safety, proper use and effectiveness standards and regulation. What this may imply is the imposition of Western standards and Evidence Based Medicine (EBM) and practices onto systems which in some cases are so removed from the Western mindset that to “regulate” them by the imposition of Western standards may actually damage these traditions.
In Point 3, despite the unfortunate use of the term “capitalising”, the concept of universal healthcare remains one of humanity’s greatest objectives but how can you ensure users make informed decisions if not by using EBM?
Evidence Based Medicine
In order to put this argument into context, let us consider what is understood by the term EBM? Firstly, the term can be read a number of different ways, though the main principles came to the fore in the early 1990s when Guyatt introduced the term “scientific medicine” and later in 1991 began to promote the term evidence-based medicine (Sur & Damh, 2011). The main idea is that a medication should be exposed to a rigorous clinical trial where it can be compared against a placebo. In a trial featuring two study groups one is given the new drug, another a dummy pill. Neither group know what they are being given. After the trial both groups are analysed for safety, efficaciousness and effectiveness. Where there any adverse effects in one group, did the new drug work better than the placebo group and, if so, how effective was it statistically speaking?
The placebo effect is well accepted. Some people get results despite not taking a recognisable therapeutic substance. The power of belief however cannot effectively be measured, so often it is assumed that a placebo effect will occur in around 30% of cases. Therefore, the new drug must be better than placebo, and hopefully with limited adverse reactions. The concept behind such trials is that they eliminate bias in an attempt to be objective.
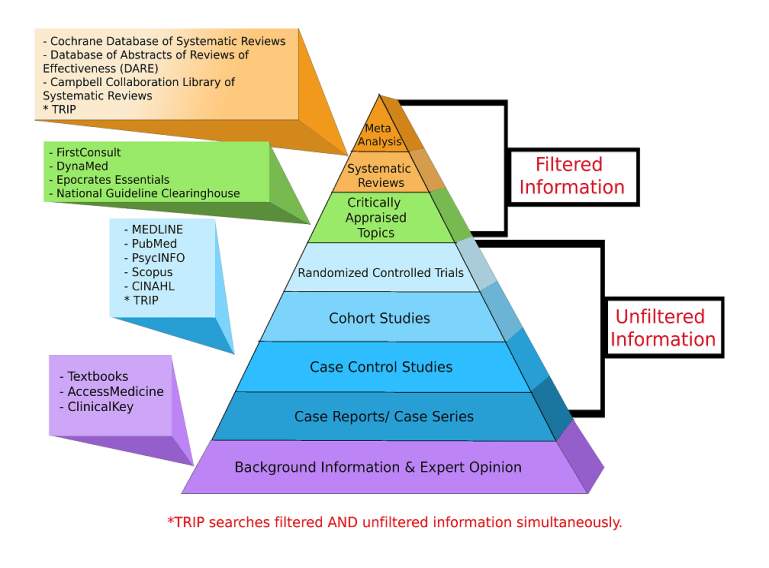
When several trials have been conducted, a systematic review or meta-analysis produces a report which summarises the results of several trials into the same drug. Such reports are considered to be the pinnacle of evidence, and are encouraged for clinical decision making. Today, we have what in some quarters is called a “Hierarchy of Evidence”. Within this hierarchy Systematic Reviews and Meta-Analysis are at the top, while traditional systems of knowledge can be found at the bottom, if they are included at all. The general evidence base is dominated by randomised clinical trials (RCT) and research-based approaches. An example of one such model by Murad et al (2016) published in the British Medical Journal (BMJ)
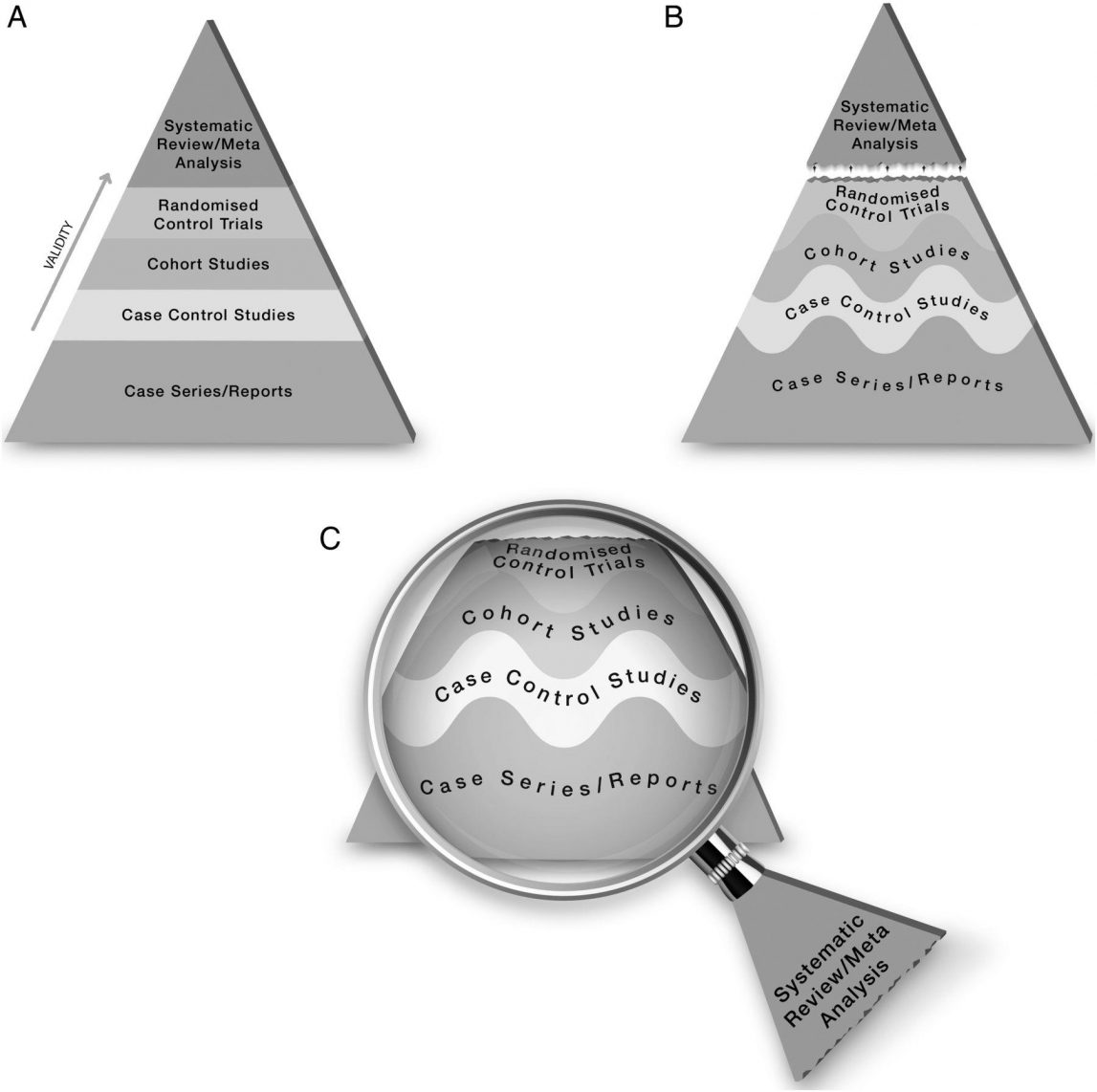
The proposed new evidence-based medicine pyramid. (A) The traditional pyramid. (B) Revising the pyramid: (1) lines separating the study designs become wavy (Grading of Recommendations Assessment, Development and Evaluation), (2) systematic reviews are ‘chopped off’ the pyramid. (C) The revised pyramid: systematic reviews are a lens through which evidence is viewed (applied) (Murad et al., 2016)
The problems with this system are multiple, yet the system is sued to bring new drugs to market and to make healthcare-legislation. The system was established to trial drugs and is perhaps appropriate to the Pharmaceutical Industry. This is because a drug is generally created to have an effect on a particular system in the body. It is therefore easy to monitor this single desired effect, how well it works and how safe it is. However, in traditional medicine herbs have multiple systemic effects, and herbal formulas have even more systemic effects. It is therefore difficult to get a measure of herbs within such a system. But there are other confounders:
- What exactly is under study? The Herb itself, or a perceived ‘active ingredient’?
- What is the actual research question being asked?
- Exactly what type of preparation is used in the study – dried herb, fresh herb, tincture or other preparation?
- Where was the starting material obtained from? How was the preparation made? How was it stored?
- What dose of the preparation was used and on what basis was the dose decided? How was the dose administered and for how long was it used?
- What sample size was used in the study and how representative of the general population is it?
- What inclusion and exclusion criteria were used for the study participants?
- Did the participants undergo any tests, such as liver function status, before taking part in the trial? Were they accessed for co-morbidities?
- Were all medications, OTC drugs or recreational drugs concurrently used recorded and taken into account?
- How sound was the internal validity of the trial? What did researchers do to eliminate bias?
- Who is conducting the trial and have they declared all interests?
- Was ethical approval granted and if so by whom?
- How does the RCT mirror real world situations? What about external validity?
- How were the statistics assessed? Which model or models were used?
- What language was used to describe the results? How were adverse reactions accessed?
- Has the RCT been repeated? Is there other qualitative data to support the results?
First of all, clinical trials often take place in specialised clinics or universities in contrived situations which do not mirror the real world. They are said to lack external validity because they are not reflective of how medications might be taken in the living world with all its variables. When you understand how to read research, particularly in relation to herbal medicine, it is common to find some or all of the above questions pertinent.
Trials can be rigged in many ways. Statistic analysis of trials may be flawed. Secondary and tertiary research may be based on flawed primary research and so on. At the root of this system, is the idea of measuring things. If we can get a measure of something by eliminating bias from our research then we can “Know” the truth.
What This Means for Traditional Medicine
The practitioners of traditional medicine have been using the same plants as their ancestors since before records began. They know what does or doesn’t work, and they have no need to have their remedies exposed to RCTs and evidence-based medicine. What the proponents of EBM fail to appreciate is that the concept of EBM is deeply patronising, for it suggests that before this system became prominent there was no evidence. It is deeply insulting to tell a herbalist their remedy doesn’t work until it is proven to work by this Western Pharmaceutical system. It is condescending to tell the patient who has repeatedly benefitted from the remedy that it may not work until it has been proven to work.
At the root of this problem is philosophy. The philosophy of EBM is based on a concept called Positivism. I want to show that if WHO wish to integrate traditional medicine into a modern healthcare system then they must first address the philosophical dictatorship of EBM. When this problem is considered it actually shows that we may have even more problems than we thought. There is therefore a risk that the WHO Traditional Medicine Strategy may misrepresent traditional medicine and may actually erode the traditional knowledge base.
The concept of Tacit Knowledge was introduced by Michael Polanyi when he began to realise that there are different types of knowledge. If what Polanyi says is true then EBM is nothing more than a medical dictatorship that may be doing more harm than good.
Introduction
What is Tacit Knowledge? Tacit knowledge is the kind of knowledge that cannot be verbalised, written down, learned from books or taught in the conventional sense. Tacit knowledge can only be experienced through direct interaction with phenomena over time. I cannot teach you tacit knowledge, and tacit knowledge cannot be codified on computers, or in articles like this.
How might tacit knowledge relate to herbal medicine? In this article I hope to use concepts from philosophy and anthropology to reveal that such a type of knowledge not only exists, but plays a far greater role in our overall knowledge and life experiences, than we might think. It raises serious questions about the idea of evidence when it comes to establishing the efficacy, efficaciousness and effectiveness of herbal medicines, which regulatory authorities like the HPRA or organisations such as WHO state must be backed by scientific data from clinical trials.
What is scientific data? Is there a type of knowledge that underpins clinical trials? If so, what is it, and how does it relate to this idea of tacit knowledge? An extirpation of the concept of tacit knowledge reveals some very profound insights, which have implications for how herbal medicine is taught, how it is practiced, how it is understood – and especially how it has been sidelined because, I will argue, it is largely a tacit form of knowledge.
The crux of the WHO document is that member states must protect traditional medical knowledge as a matter of global sustainability. Biomedicine has become too expensive, and therefore there is a mounting need to preserve traditional medicine and integrate it into a modern health care system. However, because of the intriguing concept of tacit knowledge, such an integration would actually require the dismantling of evidence hierarchies for evaluating herbal medicine, which could have profound effects on medical philosophy in general.
This also raises questions about how herbal medicine is transmitted to students and apprentices, simply because the tacit cannot be taught, but must be directly experienced, and there is a distinct lack of research in the area of how herbalists create formulas (Denham, et al, 2007). Tacit knowledge raises questions about clinical practice in particular, and goes someway to providing an explanation as to how a practitioner chooses the herbs they do.
What is Tacit Knowledge?
From the outset we need to differentiate between types of knowledge. We are all familiar with explicit forms of knowledge – the stuff we learn in the classroom, from books and other familiar mediums. Such information is simple to convey for the most part, and with study becomes familiar and can be imparted to others relatively easily.
Tacit knowledge is not like this. Why is art appealing to us? We may find it difficult to verbalise what it might represent to us on an unconscious level. Body language and emotions are something we can interpret, but can we verbalise them explicitly? We often cannot find the words when we lose a loved one, for example. How do we know how to ride a bike without any prior instruction? How come scientists were unable to build a TEA laser (Transversely Excited Atmospheric) despite having complete instructions and blueprints (Collins, 1974)? In all these instances, and there are many others, tacit knowledge is our subjective experience of phenomena.

Stradivarius violins have become one of the most sought-after instruments, regularly reaching huge sums at auction. Despite manufacturers having complete instructions and knowledge of the type of wood used, nobody is able to replicate the instrument. Why?
It is because the Stradivarius family knew about wood. They watched how the weather affected wood over the seasons; they knew when to harvest and how to prepare the wood. And they listened to its acoustics. This is tacit knowledge, and only through “listening to wood” over a lifetime can one appreciate that you cannot tell someone how to make a beautiful violin, unless they too are willing to listen. In traditional medicine there is also an idea that we can gain knowledge from listening to plants.
In anthropological research, every single ancient tribal culture has eluded to the fact that they learned herbal medicine from “talking to” and “listening to plants”. This idea of having a conversation with plants does not rest easily in the Western mind set however. It suggests that plants have a voice box and can have verbal conversation with us. What we are really talking about is that the direct experience of plants, and immersion in the ecosystems of plants, creates a tacit knowledge of how to use plants medicinally, or indeed for other purposes such as constructing buildings, or making clothes.
This type of knowledge cannot be taught in the classroom. If you want to describe the actions of Althea officinalis in the body for example, how about feeling the texture of the expressed mucilage from squeezing the root – its coolness and viscous consistency enable a clearer appreciation than just being told about it. And yet its consistency is only one aspect of the whole, which can only be realised by participation and observation.
The term Tacit Knowledge was first coined by the Hungarian Philosopher of Science Michael Polanyi (1891-1976). He described all knowledge as being personal knowledge. It is our own subjective experience of reality which gives us understanding. All judgment also rests on personal decisions, and this is of particular interest as we shall see later.
Ethnobotanist Dr. William Milliken from Kew Gardens in London speaks of the Yanomami peoples of Brazil in a recent article for Survival International. He states that the Yanomami are great observers of nature, and have a complex understanding of plants and animals that allows them to survive in an otherwise difficult environment. But vitally their interaction with nature is sustainable. He describes how they are at one with nature.
All herbal traditions began in similar ways. When it comes to evaluating herbal medicines, such as is called for by the FDA, we are going to encounter tension: The FDA states for example:
“The herbal product, which would be a “biologically based practice” insofar as CAM domains are concerned, would be a “drug” under section 201(g)(1)(B) of the Act because it is intended for use in the diagnosis, cure, mitigation, treatment, or prevention of disease in man. The same herbal product would also be a “new drug” under section 201(p)(1) of the Act unless it is generally recognised, among experts qualified by scientific training and experience to evaluate the safety and effectiveness of drugs, as safe and effective for use under the conditions prescribed, recommended, or suggested in the labelling” (FDA, 2006).
In other words, only experts qualified by scientific training can evaluate herbs intended as medicines, usually by the use of randomised controlled trials and systematic literature reviews. But this is not how herbs were traditionally evaluated, and therefore what we see here is an attempt by those enthralled to the scientific model to codify the tacit knowledge of traditional medicine cultures. The problem of course is that you cannot codify tacit knowledge.
In regards to traditional medicine tacit knowledge is a distinct form of knowledge, born out of a need for survival in difficult environments (Sternberg, et al, 2001). It is a matter of adaptation by both participation and observation, which allows people to live deep in jungles or high in the mountains, where the interaction between animals and plants and the weather creates a series of associations and meanings which are very difficult to articulate.
This suggests that people compare their health with observation of varying extremes of weather patterns, hot and cold, usually within an animist cosmology (Lewinsohn, 1998). Animism is the idea that all things are alive and moving, even mountains. Names are given to these things which in turn have associations. For Tabwa practitioners in the Congo the preparation of herbs involves analogies between human bodies and trees so feet, torso and head correspond with roots, trunk and branches respectively. Plant runners (stolons) are similarly equated with the umbilicus. Some plants self-propagate with runners correlating with fertility and the umbilicus which connects one generation to the next. One lives in the environment and finds meaning in the validity of relationships between phenomena. In Tabwa the “vocabulary of pathology” is drawn from “the domain of nature” (Davis-Roberts, 1981, p. 311). Energetic systems permeate all of the great herbal systems of the world from TCM to Kampo; from Ayurveda to Unani Tibb and the Greek humoral concepts which underpin Western Herbal Medicine. But there is a tension between the world of Biomedicine and herbal medicine, which comes down to theories of knowledge. There is also tension in herbal medicine itself, between those who prefer a traditional approach to those that feel the need for scientific rigour.
The problem with “tradition” is what tradition is meant, and where does that tradition begin or end? Tradition can accept science as a tool, but rather as a good servant rather than a bad master. Science, however seems to have lost sight of tacit forms of knowledge. Why might this be important?
In order to show how this tension arises it is necessary to understand how all forms of knowledge are underpinned by a philosophy.
The Philosophy of Tacit Knowledge

Western Philosophy began in Ancient Greece. From these times philosophers tried to work out the world around them and their role in it. One of the most important philosophers was Aristotle (384-322 BCE) who studied the concept of knowledge almost 2500 years ago!
What is knowledge, where does it come from and how can we know if it is true? These were Aristotle’s central concerns. Aristotle came to accept that there were different types of knowledge. He used several separate terms for knowledge: epistēmē (to know); technē (skill) and phrónesis (practical wisdom). Phrónesis stood in contrast to sophía (theoretical wisdom) (Aristotle, 2009). Another term for a certain type of knowledge in Ancient Greece was Metis, meaning cunning. But Aristotle came to a very important conclusion at the birth of Western Philosophy: All knowledge comes from perception!
This is important to our discussion. Aristotle is talking about the use of the senses to gain information and knowledge. Aristotle was a major influence on the development of Western philosophical ideas, but by medieval times other philosophers were having different ideas.
René Descartes (1596-1650) would not accept that knowledge came from perception and he broke with the Aristotelian tradition. Descartes thought that if two or more people looked at the same thing, their experiences would always be different. Knowledge needed to come from a place where it could be independently verified (Descartes, 2013). In philosophy this is known as the Cartesian Shift.
Descartes had a famous phrase “I think, therefore I am”. Knowledge came from thinking, and from the use of mathematics, algebra and geometry in his world view. Therefore, if we could measure things, we could understand them and gain knowledge. The Cartesian world view was very influential in the sciences, and in medicine in particular the human body became represented as a machine, made up of working parts. In Europe such philosophy became central in the ascending science of anatomy from the 17th century onwards, particularly at the University of Padua and the anatomical teaching of Giovanni Battista Morgagni (1682-1771).
Two centuries later, in the 1920s, a group of philosophers who called themselves The Vienna Circle, proposed a new development of the Cartesian world view, which is called Positivism, or Logical Positivism. In this system knowledge is only true if it can be verified by logic and mathematics. The verification principle, as it was called, means that knowledge can only be true if we can measure it. If something was considered metaphysical, and could not be measured, it was considered by the Positivists to be untrue (Ayer, 1959).
This becomes important to our discussion, for what is really being said here is that explicit or measurable forms of knowledge are true, and tacit knowledge is untrue, because it cannot be verified. This does not mean that tacit knowledge doesn’t exist, only that it cannot be verified according to the rules set out by Positivism.
These philosophical underpinnings become pivotal when we consider the recent development of Evidence-Based Medicine (EBM). Central to EBM is the Positivist approach to knowledge. EBM has its origins in the early 70’s, but by the 1990s it became the dominant trend in biomedicine and, by extension, in health care legislation.
Clinical decision-making must be based on best evidence from systematic research, according to the advocates of EBM. In other words, you have to measure a medicine, by isolating perceived “active ingredients” and using randomized clinical trials to demonstrate their efficacy, effectiveness and safety. Yet in the EBM system, expert opinion is actually at the bottom of the evidence hierarchy. Herbalists are only too aware of what this means when it comes to evaluating herbal medicines within this set of rules. But when we consider that this set of rules is designed so that it literally excludes tacit knowledge, we begin to see the problems. We must bear in mind that just because a set of rules cannot measure tacit forms of knowledge, does not mean that tacit knowledge does not exist.
It is also worth keeping in mind one of the most quoted definitions of EBM:
“Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. Increased expertise is reflected in many ways, but especially in more effective and efficient diagnosis and in the more thoughtful identification and compassionate use of individual patients’ predicaments, rights, and preferences in making clinical decisions about their care” (Sackett, et al, 1995).
The last sentence is especially important. It concerns what is known as patient centred care, and I will consider it in greater detail later in the text.
Philosophical Conundrums
A number of philosophers have challenged the rules of Logical Positivism, and developed counter arguments which expose the Achilles’ heel of the Positivist philosophy.
The Austrian philosopher Christian Von Ehrenfels (1859-1932) developed a concept called gestaltheorie. Gestalt is about looking at shapes from the perspective of wholeness. If we only look at part of shape, then we cannot see its wholeness (Von Ehrenfels, 1890). If we take a square made up of 4 lines and look at the lines in isolation, we miss its square-ness. Gestalt became a very important development in psychology, but it also led other philosophers to consider the idea of wholeness.
The German philosopher Edmund Husserl (1859-1938) developed a concept called phenomenology, which was a major influence in 20th century philosophy. Phenomenology questions the rules of logical positivism. You cannot measure someone’s consciousness it suggests. You cannot work out a mathematical formula that can capture what a human being is feeling (Husserl, 2012). These concepts were developed by the French philosopher Maurice Merleau-Ponty (1908-1961). Merleau-Ponty wrote about the visible and the invisible, two things which merge to form our consciousness. He means both our objective and subjective experiences of reality are necessary for knowledge. While the Positivists saw only objective experiences as being true (because they could be measured), the phenomenologists said that the subjective was an essential component. Merleau-Ponty called this “embodied knowing”.
The British philosopher Gilbert Ryle (1900-1976) also challenged the objectivity of Positivism. He is famous for the phrase the Ghost in the Machine. If the human body is just a machine made up of working parts like the cogs and wheels of a clock, then where is the mind, he challenged? Is it simply a spirit tethered to the machine? In philosophic terms this represents what is called a category mistake. Ryle puts it this way – suppose you show me the libraries, halls and colleges which make up the university, yet I cannot find the university itself?
To put it another way, can you isolate what you believe to be the active ingredients of a rose, and then claim to know all the medical qualities of the rose? This is a category mistake, and it happens daily in medical research into herbal medicine. Ryle called this the “bogey of mechanism” (Ryle, 2000).
Ryle also offered a second philosophical conundrum in regards to Positivism, which in philosophy is known as the regress argument. And it is a petty damning argument, but is best illustrated by perhaps the most important philosopher of the 20th century, Ludwig Wittgenstein (1889-1951).
Wittgenstein was very interested in rules about knowledge, but he became fixated on the idea of where rules begin and end. He used the analogy of two tribesmen playing a game of chess to illustrate his quandary. The tribesmen are familiar with the strategy of chess but also yell and shake their fists at each other, and stomp their feet. Are they necessarily breaking the rules of chess by yelling and stomping their feet? What happens in a situation when something is both in accord and against the rules at the same time? In such an instance we need to consider the limitations of having rules about knowledge. Wittgenstein called this a language game. If there are two ideologies which disagree, one ideology dominates, often through persuasion. Wittgenstein puts it in terms of missionaries converting tribes to their beliefs, often by force.
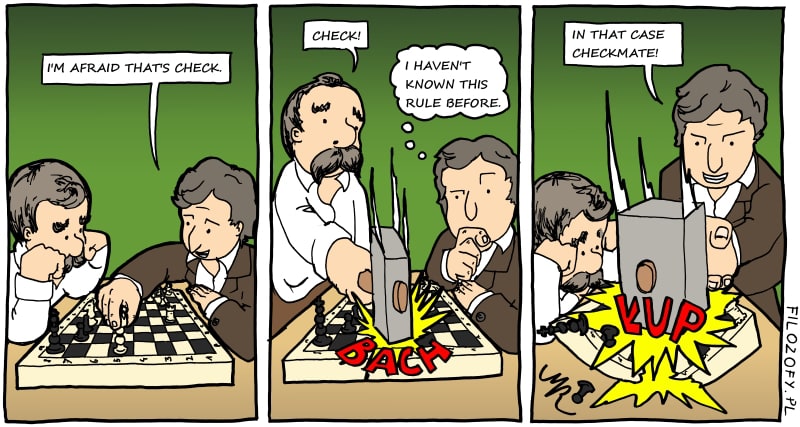
The problem is that if you make rules about what does or doesn’t constitute knowledge you end up with infinite regress. The regress argument in philosophy suggests that if you can challenge the rules indefinitely then the rules are finite, they are not the definitive account of knowledge. Using rules, which are endlessly questionable, is logically indefensible.
Tacit Knowledge is Personal Knowledge
These developments in philosophy influenced the Hungarian philosopher Michael Polanyi (1891-1976). Polanyi coined the term tacit knowledge in 1958, to show the difference between different types of knowing, but importantly to reveal that science had become exclusive by rejecting the personal experience simply because it could not measure it. Life, said Polanyi in 1968, has “an irreducible structure”! Polanyi was concerned that Positivism, which promised complete objectivity in the exact sciences, was a delusion because personal judgment, which cannot be quantified, is always involved in “applying the formulae of mechanics to the facts of experience” (Polanyi, 2013, pp. 18-19).
Polanyi was a powerful influence on two other philosophers, who saw the difficulties associated with making rules about knowledge. Thomas Kuhn (1922-1996) drew on the theory of tacit knowledge, and from him we have the concept of the paradigm shift. Science does not progress in a linear fashion, but rather a group of scientists agree on a certain way of doing things and achieve consensus (Kuhn, 2012). A paradigm shift occurs when consensus breaks down and new theories take prominence. In today’s society paradigms are often influenced by money, rather than science.
The Austrian-American philosopher Paul Feyerabend (1924-1994) also questioned positivism through the theory of classic anarchism. Positivism was simply dogma to Feyerabend, propped up by commercial interests. For Feyerabend modern science follows a paradigm (Positivism) which employs a set of rules. But he says witchcraft employs a paradigm also, so if we say knowledge is defined by rules then all and any set of rules have equal value. All belief systems are valid, with one caveat: The difference between any set of rules is in its practical outcomes. It does not matter what we believe, or what terms we use to describe our beliefs, but rather if they are practical or not. In medicine, if follows, that whatever system we employ is actually irrelevant. What is relevant is whether or not that system produces positive outcomes. Philosophers looking for ‘machinery’ which works in ideal conditions fail to concern themselves with how this ‘machinery’ will work in reality, Feyerabend maintained. How are scientists going to deal with their actual surroundings? Such enquiry will have to be anthropological (Feyerabend, 2010, p. 204).
The Anthropology of Tacit Knowledge
Ethnobotany is a particular field of medical anthropology which concerns human relationships with plants (Singer & Erickson, 2011). Medical anthropology examines cultural interpretations of health and illness in complex pluralistic societies where multiple strategies are employed to tackle health issues (Salkeld, 2014). In the parlance of anthropology such phenomena are considered from either an emic or etic perspective.
These terms are an analogy on the linguistic terms phonetic and phonemic promoted by the American anthropologist and linguist Kenneth Pike (1912-2000). Pike believed these terms are adaptable to any human behaviour, for example phonemics is the subjective meaning and understanding of the sound of language, whereas phonetics is the objective study of these sounds. An emic approach therefore considers generalised phenomena from culturally-patterned behaviour whereas the etic analysis considers phenomena peculiar to a specific language or culture (Pike, 1954).
Emics refer to how people think and gain meaning within their native cosmology, for example towards the medicinal use of plants. Etics proffers an objective rendering of emic observations; the outsider looking in and interpreting how plants might be used more universally. This dichotomy creates tensions. Anthropologists can erroneously interpret phenomena if “the objectives of one explanatory system are substituted by the objectives of another”; further complicated if the interpreter invokes scientific “rules of conduct” to try to debunk the other (Fisher & Werner, 1978, p. 194). Jardine considers the limits of emic interpretation and etic analysis. He argues “articulation of tacit knowledge” has been central to the discussion between emic and etic (Jardine, 2004, p. 243).
Bolton (1995) contends anthropologists cannot experience what others experience because they aren’t integrated politically, historically or practically into the host society. As an outsider the anthropologist therefore cannot be neutral and this inclines her towards a hermeneutic representation of spectacle; a language-game as Wittgenstein would have it. Frankel and Lewis (1988)argued that anthropological studies of traditional medicine have tended to be more concerned with beliefs than actual practice.
An anthropological study relies upon differentiating between communicable and hidden forms of knowledge. However, Rajpramukh (2007) believes an etic perspective must also contain an emic component reflecting the tradition from which the anthropologist originates! Jardine concludes that “emics without etics is blind” while “etics without emics is empty” (Jardine, 2004, p. 275).
If we adopt Jardine’s approach it becomes pertinent to consider that emic knowledge has ties to tacit knowledge, because some emic knowledge cannot be verbalized (Kaasbøll, 1995).
For example, in Cherokee tradition Deer medicine is associated with rheumatism. In Cherokee mythology the animal persons held conference and decided they’d had enough of human abuse. They conspired to create disease to keep humans in check. To the deer people any Indian who killed a deer without asking pardon, reasoning that they needed to kill because they were starving, would be afflicted with pain in their joints so they could no longer hunt deer. The plant people were concerned with this turn of events and offered themselves as cures to these illnesses. The tale is cautionary and concerns sustainable use of resources but what else might it imply?

An etic approach might consider the Cherokee discovered deer medicine because they noticed that deer were very nimble creatures, and by watching what plants deer eat they could infer what to use for illnesses were nimbleness was checked. Herbs were given names such as deer’s eye, deer shin or deer’s tongue and could be used in a formula for rheumatism. But the Cherokee observe all nature and also gain information from plant people. This may seem more difficult to articulate in etic terms and could be easily seen as a belief rather than a valid and practical art. The question is whether or not this knowledge has practical outcomes. Modern research shows deer’s tongue (Liatris odoratissima)contains coumarins which are anti-inflammatory and possibly immune-regulating, which would be appropriate for arthritis (Kontogiorgis & Hadjipavlou-Litina, 2005).
For many native cultures the language of plants is a practical art developed from interaction with nature over millennia. Information is gleaned from a plant’s location; colour; scent; taste; feel and other characteristics comparable with the European Doctrine of Signatures. Paracelsus, with whom the doctrine is associated, writes “Nature marks each growth … according to its curative benefit” (as cited in Breverton, 2011). The doctrine of signatures has received a limited reading in European research (Saupe & Sharpless, 2007). A plant is only considered for morphological characteristics which resemble a body part, but if we bring in the wider perception of the senses other information can be gleaned.
Location offers information. A bog plant, like Apium graveolens, can remediate or increase damp conditions; a plant growing at altitude like Ligusticum porteri can relieve altitude sickness. Smell offers information. The scent of Gaultheria procumbens indicates pain-relief (modern research will talk of methyl salicylates). Colour and taste offer further information but it is the merging of all these phenomenal experiences which creates practical knowledge. The combination of sensory information is regarded as a communication between plants and humans from which tacit knowledge evolves.
Foreman (1849) believed Cherokee medicine was not a study of curious enquiry but should be treated as a subject of the deepest interest. This contrasts sharply with Mooney (1890) who stated Cherokee medicine can never be compared with that practiced by white physicians. This shows the contrast of emic and etic viewpoints in early ethnobotanical studies of Cherokee medicine. And it is a similar situation to what we saw in philosophy when one rule supersedes another.
Mooney (1890) thought it wrong to see the Indian healer’s knowledge outranking that of the white physician. The white physician, he maintained, has studied under experts while the Indian healer “at best can only consult with a few brother shamans” and his knowledge is on a par with the average white farmer’s wife (Mooney, 1890, p. 44). Such were the condescending tones that disgraced many early ethnobotanical studies. Mooney spent three seasons with the Cherokee learning about herbs and the ceremonies accompanying them yet he continually castigates the Cherokee comparing their, in his eyes, limited botanical knowledge with that of white botanists. In Mooney’s narrow opinion herbs are chosen due to some “fanciful connection” between plants and animal spirits. A person with rheumatism would be given deer medicine along with a prayer evoking the natural enemies of deer, such as dog spirits, who will come and drive out the deer spirit. This is a clear example of etic opinion dismissing emic perspective because it didn’t fit the (then) Eurocentric position.
Knowing and Not Knowing Life
Etkin (1986) opines that research into herbal medicine needs a multidisciplinary approach. Research which incorporates relationships between medical cosmologies and perceptions of the living world, for example the use of herbs by an indigenous culture like the Cherokee, are sharply contrasted with modern disciplines such as botany and pharmacology whose cold scientific terminology may be devoid of cultural and contextual data. She describes this contrast in terms of ethnobotany and ethnopharmacology as being “botanically uninformed” and “anthropologically naïve” (Etkin, 1986, p. 2).
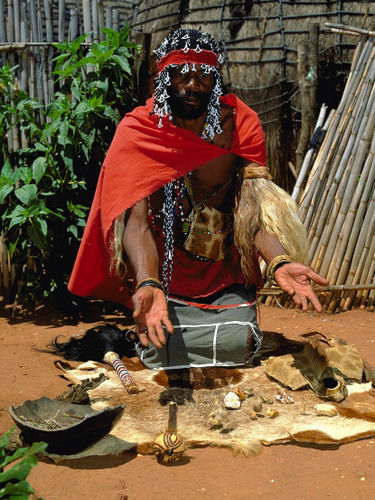
To illustrate differentiations in ‘knowing’ Laplante (2014) examined the contrasts between knowing ‘life’ from the perspectives of molecular biology with traditional perspectives of Xhosa medicine in South Africa. In a preclinical trial experts from both systems collaborated on preparing a local plant for a RCT. Both biologists and healers shared common interest in the hope of bringing healing. The biologists were looking for an agent to check tuberculosis by inhibiting the bacterium at the molecular level. The Izangoma healers offered clues as to what plants might contain such agents; but in their own medical ‘knowing’ they were more concerned with altering bodily processes to generate resistance to the tuberculosis bacterium. From these differing perspectives Laplante argues that the use of the RCT is both a way of ‘knowing’ and ‘not knowing’ life at the same time (Laplante, 2014).
The biologists and the Izangoma ‘know’ their areas of expertise and are attuned to their respective worlds. This raises the issue of ‘not-knowing’ the ‘other’. Merleau-Ponty assumes mind and body are in “continuous entanglement”and contrasts ontology from the perspective of the body alone and from the body-mind entanglement. The world is already there before we begin to reflect upon it (Merleau-Ponty, 2014). The RCT therefore presents a way of knowing and not knowing life simultaneously. RCTs generates precise knowledge of biological mechanisms and pathways within a closed environment, but at the cost of losing sight of their “interweaving in mediums” (Laplante 2014, p. 3). Philosophically and anthropologically speaking the RCT does not seem to be an appropriate method for gaining medicinal knowledge of plants. This creates tension.
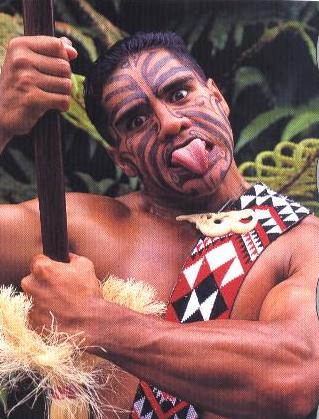
To understand traditional medicine does the researcher need to become similarly grounded? Harvey (2004) suggests that an alternative relational approach is needed to avoid tension. He explores the notion of guesthood with the Maori. Visitors attend a meeting house (whare), which is also an ancestor house situated in a significant place (marae atea). To enter the whare is to enter the community. Only a descendent can enter a whare with impunity. Visitors may enter if they meet the protocol for guests. A woman invites a visitor in but a warrior places a symbol of war (taki) in their stead and performs a haka (warrior posture). The visitor is expected to pick up the taki to symbolise respect rather than attack the warrior and by this they accept the roles of guesthood. Strangers must then give reasons for visiting and if things go well food can be shared. Being a guest is different than being a visitor for the guest recognises the sovereignty of the host, and importantly their intellectual property (Harvey, 2004). Guesthood demands researchers seek a common ground and recognise the priority of their hosts (Hume & Mulcock, 2013).
Patient Centred Care?
Earlier we looked at EBM and patient-centred care. Anything which cannot be measured remains outside Positivist concern. This doesn’t mean something beyond its measure doesn’t exist or is irrelevant. EBM has led to a “critical appraisal of therapeutic knowledge” however this must involve an “ethical approach” towards patient-centred care (Kruger, 2010, p. 69). This patient-centred care requires an appreciation of patient narrative which is a tacit experience. How then might EBM accommodate a patient’s tacit knowledge?
A combination of clinical expertise, systematic research and patient values underpin EBM yet without a holistic approach practice can become “tyrannised by evidence” (Sackett et al., 1996, p. 72).
Husserl found the need to develop a new field of knowledge to overcome the conundrums thrown up by Positivism, which he termed transcendental subjectivity – an independent realm of direct experience(Husserl, 2012). Husserl’s method, the study of “that which appears“, is known as phenomenology. Küpers (2005) believes that in understanding the differences between concepts of knowledge the researcher needs to understand the life-world of the subject under scrutiny. Those involved in their life-worlds are “embodied”beings experiencing “lived situations“ (Merleau-Ponty, 1968). Our living body, then, experiences reality only in the way we affect it or it affects us – and therefore we are grounded within it (Küpers, 2005).
In a clinical situation the practitioner enters the life world of the patient and listens for many voices. the term polyphony refers to all the different voices that make up a choir. The herbalist picks up on each voice and allows their tacit experience to recognise patterns and to choose suitable herbs which fit the patient’s predicament. In this sense a holistic approach is more congruent with the patient’s tacit experience of life and illness than the reductionist approach which only sees their illness. Knowing and not knowing life at the same time!
Earlier we looked at the triangle of evidence hierarchy under EBM, where expert knowledge was placed at the bottom of the triangle. In order to embrace the oft-touted patient centred care, practitioners use their expertise as if it were at the top of the triangle, because the tacit approach to consultation embraces the patient’s subjective experience, and uses time-honoured herbs accordingly.
Professor Tim Thornton argues that tacit knowledge is the unifying factor in Sackett’s tripartite division of EBM. If clinical experience underpins the use of best evidence, then best evidence must also include clinical judgment. This judgment cannot be based solely on best evidence but must also incorporate values, such as patient centred care, Thornton contends. Ethical values cannot be codified, and are therefore tacit, but ethical judgments do involve validity. Judgment cannot be solely based on rules, Thornton argues, and yet common interpretations of EBM often discount expert opinion (Thornton, 2006). It is argued that practice based solely on clinical trials and reviews has depersonalised healthcare. They contend that “no explicit concern with the multiple other dimensions of human suffering, illness, fluctuating and functioning has ever been convincingly demonstrated by EBM” (Miles & Asbridge, 2014, p. 135).
WHO Traditional Medicine Strategy
What is traditional medicine? Usually it is a system based on elemental or humoral concepts. Earlier we considered the WHO’s Traditional Medicine Strategy which is to preserve traditional medicine as a matter of urgency and global sustainability in times of food crises, climate change, antibiotic resistance and mounting austerity. Biomedicine has become too costly and unwieldy to have international presence. 80% of the world population uses herbal medicine as their primary source of healthcare (WHO, 2007). It makes sense to preserve systems of medicine where biomedicine does not or cannot reach. WHO talks about codifying traditional knowledge and integrating it into a modern health care system, yet the tacit cannot be codified, and therefore traditional medicine actually becomes at risk of being lost? We cannot codify or prove traditional medicine using clinical trials and evidence hierarchies. This is simply another case of etics dominating emics, of one set of rules dominating another, which is philosophically and anthropologically unsound.
If WHO are serious about this strategy, then the Maori concept of guesthood offers a route forward. If traditional practitioners are considered as experts, then they need to be treated as such. Guesthood offers a concept whereby researchers can approach another culture from a position of respect (Harvey, 2004). They do not need to prove their system of medicine by trying to ingratiate it into the EBM model. And yet this has happened in the UK, which in consequence has seen a decline in herbal degree courses; and many graduates turning to TCM or Ayurveda because their teaching lacked an energetic approach so fundamental to tradition. I find many student graduates to not last long as practitioners because they are missing the key energetic holism that permeates the core of traditional herbal medicine.
There is another fundamental aspect to all of this. To neglect tacit knowledge may actually be a breach of medical ethics. Beauchamp and Childress (2009) raise the issues of respect for autonomy, nonmaleficence, beneficence and justice as the cornerstones of biomedical ethics. By solely using clinical trials as best evidence researchers run the risk of not respecting autonomy by failing to incorporate the evidence of a patient’s experience and values. These experiences are often tacit. This can challenge the concepts of nonmaleficence and beneficence because a limited evidence base can leave room for error. If herbal medicine remains marginalised as a consequence this feeds into the concept of Justice, due to a potential inequality in access to herbal healthcare by misrepresentation. In light of the increasing burden of chronic disease and the controversy of iatrogenesis can we afford to ignore tacit knowledge?
Conclusions
The concept of tacit knowledge provides a way of showing that there are different forms of knowledge. In the field of medicine especially, it reveals the epistemological tensions which have led to a medical dictatorship in the West, which has left herbalists marginalised and misunderstood. In order to bring herbal medicine back into the public domain I feel we need to use tacit knowledge to explain how evidence hierarchies are damaging to non-explicit forms of knowledge, and are philosophically, anthropologically and ethically problematic.
In order for WHO to implement the preservation of traditional medicine, they need to work directly with herbalists and create a true healthcare system, where the patient has the right to choose their medicine. This can only happen when it is understood that health itself is a tacit experience, and patient centred care must embrace it. This can only happen when holistic approaches which can incorporate patient’s subjective experiences are brought center stage.
This concept also shines a light on herbal medicine. It shows that all paths are valid if they can make people well again.
Plant Healer Federation is an experiment. I have been making contact with professional associations and tribal representatives and asking them to join in the dialogue and give voice to concerns over the Traditional Medicine Strategy. A unified voice which speaks for international concerns could avoid the risk of WHO members implementing an undesirable strategy such as insisting on systematic research to validate traditional medicine.
PHF has a private website with a built-in translator of over 80 languages, where representatives of organisations from all over the world can speak on behalf of their tradition, and reflect back to their members or tribe. Given the size and scope of this experiment it was thought necessary to initially limit PHF to professional organisations or tribal representatives with a maximum of 5 persons per organisation to avoid one group becoming dominant.
The online forum also allows the sharing of resources – information about events in different countries, translation of research or textbooks, speaker and student exchanges and the creation of case series library. We are also working towards an international event which will move from country to country, with the first event planned for Majorca in 2020.
In time PHF will become open to individuals but the main aim now is to encourage ways of sharing and to work on a reply to the WHO Traditional Medicine Strategy, and give traditional herbal medicine an international voice in uncertain times.
www.planthealerfederation.com
“And the youth became silent for a while as if he would learn speech from the murmur of the river and the rustle of leaves on the boughs”.
(Kahlil)
References
Ayer, A. J. (Ed.). (1959). Logical positivism. New York, NY, USA: Simon and Schuster.
Beauchamp, T. L., & Childress, J. F. (2009). Principles of biomedical ethics. (6th ed.) Oxford, UK: Oxford University Press.
Bolton, J. (1995). Medical practice and anthropological bias. Social Science & Medicine, 40(12), 1655-1661.
Breverton, T. (2011). Breverton’s complete herbal. London, UK: Quercus.
Collins, H. M. (1974). The TEA set: Tacit knowledge and scientific networks. Science studies, 4(2), 165-185.
Davis-Roberts, C. (1981). Kutambuwa ugonjuwa: concepts of illness and transformation among the Tabwa of Zaire. Social Science & Medicine. Part B: Medical Anthropology, 15(3), 309-316.
Denham, A., Green, J., & Hawkey, S. (2011). What’s in the bottle?: prescriptions formulate by medical herbalists in a clinical trial of treatment during the menopause. Journal of Herbal Medicine, 1(3), 95-101.
Descartes, R., & Cottingham, J. (2013). René Descartes: Meditations on first philosophy: With selections from the objections and replies. Cambridge University Press.
Ehrenfels, C. V. (1890). Über gestaltqualitäten. Vierteljahresschrift für wissenschaftliche Philosophie, 14(3), 249-292.
Etkin, N. L. (1986). Multidisciplinary perspectives in the interpretation of plants used in indigenous medicine and diet. In N. L. Etkin (Ed.). Plants in Indigenous Medicine and Diet: Biobehavioural Approaches. (pp. 2-29).London, UK:Routledge
Evans, S. (2008). Changing the knowledge base in western herbal medicine. Social Science & Medicine, 67(12), 2098-2106
Frankel, S., & Lewis, G. (1989). A continuing trial of treatment: medical pluralism in Papua New Guinea. Springer Science & Business Media.
Feyerabend, P. (1987). Science in a free society. (2nd ed.) London, UK: Verso
Feyerabend, P. (1995). Nature as a work of art. In J. Götschl (Ed.) Revolutionary changes in understanding man and society: scopes and limits (pp. 255-267). Berlin, Germany: Springer.
Feyerabend, P. (2010). Against method (4th ed.). London, UK: Verso.
Fisher, L. E., & Werner, O. (1978). Explaining explanation: tension in American anthropology. Journal of Anthropological Research, 194-218.
Foreman, R. (1849). The Cherokee physician, or, Indian guide to health. Asville, NC: Edney and Dedman.
Harvey, G. (2004). Performing and constructing research as guesthood in the study of religions. In L. Hume, & J. Mulcock (Eds.), Anthropologists in the Field: Cases in Participant Observation, (pp. 168-183). Chichester, UK: Columbia University Press.
Hume, L., & Mulcock, J. (Eds.). (2013). Anthropologists in the field: cases in participant observation. Chichester, UK: Columbia University Press.
Husserl, E. (2012). Cartesian meditations: an introduction to phenomenology. (D. Cairns, trans.). Nijhoff, The Hague, Netherlands. Springer
Jardine, N. (2004). Etics and emics (not to mention anemics and emetics) in the history of the sciences. History of Science, 42, 261-278.
Kaasbøll, J. J. (1995). Knowledge from the inside and outside in participative development and research on participative development. Retrieved 5th March 2015 from: http://urn.nb.no/URN:NBN:no-14265
Kontogiorgis, C. A., & Hadjipavlou-Litina, D. J. (2005). Synthesis and antiinflammatory activity of coumarin derivatives. Journal of Medicinal Chemistry, 48(20), 6400-6408.
Kruger, M. (2010). The ethical approach to evidence-based medicine. South African Journal of Clinical Nutrition, 23(1), S69-S70.
Kuhn, T. S. (2012). The structure of scientific revolutions. Chicago, IL, USA: University of Chicago Press.
Küpers, W. (2005). Phenomenology of embodied implicit and narrative knowing. Journal of Knowledge Management, 9(6), 114-133.
Laplante, J. (2014). On knowing and not knowing “life” in molecular biology and Xhosa healing: ontologies in the preclinical trial of a South African indigenous medicine (Muthi). Anthropology of Consciousness, 25(1), 1-31.
Lewinsohn, R. (1998). Medical theories, science, and the practice of medicine. Social Science & Medicine, 46(10), 1261-1270.
Merleau-Ponty, M. (1968). The visible and the invisible: followed by working notes. (C Lefort Trans.). Evanston, IL, USA: Northwestern University Press.
Merleau-Ponty, M. (2014). Phenomenology of perception. (D. A. Landes, Trans.) (2012 ed.). London, UK: Routledge.
Miles, A., & Asbridge, J. E. (2014). Modern healthcare: A technical giant, yet an ethical child? European Journal for Person Centered Healthcare, 2(2), 135-139.
Mooney, J. (1890). Cherokee theory and practice of medicine. The Journal of American Folklore, 3(8), 44-50.
Pike, K. L. (1954). Language in relation to a unified theory of the structure of human behavior. Dallas, TX, US: Summer Institute of Linguistics. (1954). xv 255 pp.
Polanyi, M. (2013). Personal knowledge: Towards a post-critical philosophy (1962 Edition). Chicago, IL, USA: University of Chicago Press.
Polanyi, M. (2009). The tacit dimension (1966 ed.). Chicago, IL, USA: University of Chicago Press.
Rajpramukh, K. (2007). Anthropological dialectics in illness and indigenous knowledge. Anthropologist Special Review, 3, 51-57
Ryle, G. (2000). The concept of mind. London, UK: Penguin Classics.
Sackett, D. L., Rosenberg, W. M., Gray, J. A., Haynes, R. B., & Richardson, W. S. (1996). Evidence based medicine: what it is and what it isn’t. BMJ: British Medical Journal, 312(7023), 71
Salkeld, E. J. (2014). Framework negotiations: diagnostic insights among alternative medical practitioners participating in integrative medicine case conferences. Medical Anthropology Quarterly, 28(1), 44-65.
Saupe, S. G., & Sharpless, K. E.. (2008). Solution to “doctrine of signatures” challenge. Analytical and Bioanalytical Chemistry, 390(-), 79-83. doi:10.1007/s00216-007-1743-8
Singer, M., & Erickson, P. I. (eds.) (2011). A companion to medical anthropology. Chichester, UK: Blackwell/John Wiley & Sons.
Sternberg, R. J., Nokes, C., Geissler, P. W., Prince, R., Okatcha, F., Bundy, D. A., & Grigorenko, E. L. (2001). The relationship between academic and practical intelligence: A case study in Kenya. Intelligence, 29(5), 401-418.
Thornton, T. (2006). Tacit knowledge as the unifying factor in evidence based medicine and clinical judgement. Philosophy, Ethics, and Humanities in Medicine, 1(1), 2.
Wittgenstein, L. (2009). Philosophical investigations. (G. E. M. Anscombe, & P.M.S. Hacker trans.). Chichester, UK: Wiley-Blackwell.
World Health Organization. (2015). WHO traditional medicine strategy 2014–2023. 2013. Geneva: World Health Organization.