Have you ever laid awake in a state of abject torture with legs that simply cannot stay still?
The uncontrollable flick of the leg, twitch of the thigh, the need to move! Restless legs can come and go but tend to get more frequent with age. It’s one of those sort of functional things that may get diagnosed, but no real answers given as to what causes it or how you can help eliminate it.
No matter how hard you try to relax and breathe or meditate, your legs will not rest. It can be so frustrating even though it seems a simple thing. The irritation can impact sleep, and leave you feeling drained and exhausted. We wanted to share a bit about what can cause restless legs and how you might be able to soothe the symptoms of restless leg syndrome and support your system.
History of RLS
Restless Leg Syndrome (also called Willis-Ekbom Disease) was first medically recognised in the 17th century. In the last 50 or so years, there has been more interest in how overall health and lifestyle can positively impact health. On the back of this, restless legs have been studied in more depth in these last decades. Restless legs are mainly felt during quiet wakefulness and getting to sleep.
 In 1672, Thomas Willis, an English physician, published what is considered the earliest English work on medical psychology. He was an early pioneer of the mind-brain connections and influences on the very nature of being that have become prominent in present-day neuropsychiatry and philosophy of mind. The earliest description of restless legs associated with sleep problems was probably by Sir Thomas Willis (1672). He produced a case report on restless legs in 1685 and has subsequently been included in the name of the syndrome. His life actually overlapped with Renee Decartes, who is often blamed for the separation between mechanistic and holistic medical models. Decartes’ work was simplified into this binary ideology but in reality, it was much more nuanced. It’s said that he became a scapegoat for the medical model that was arising where mechanisms fitted the medical paradigm and research that was coming into effect.
In 1672, Thomas Willis, an English physician, published what is considered the earliest English work on medical psychology. He was an early pioneer of the mind-brain connections and influences on the very nature of being that have become prominent in present-day neuropsychiatry and philosophy of mind. The earliest description of restless legs associated with sleep problems was probably by Sir Thomas Willis (1672). He produced a case report on restless legs in 1685 and has subsequently been included in the name of the syndrome. His life actually overlapped with Renee Decartes, who is often blamed for the separation between mechanistic and holistic medical models. Decartes’ work was simplified into this binary ideology but in reality, it was much more nuanced. It’s said that he became a scapegoat for the medical model that was arising where mechanisms fitted the medical paradigm and research that was coming into effect.
Who can get RLS?
The symptoms of restless leg syndrome can affect people of any age or gender, although its onset is more prevalent in middle age and it tends to affect considerably more women than men. In fact, reported cases are twice as common in women than in men. This is not thoroughly understood, but may be because of higher levels of oestrogen, or rather changes to oestrogen levels, than the level of oestrogen itself, that can trigger RLS.
However, RLS frequently emerges during pregnancy, especially in the third trimester when oestrogen levels are particularly high. In addition, many women suffer from relative iron deficiency during this time, and iron deficiency in specific parts of the brain has been shown in RLS. Women’s iron stores are always lower than men’s because of monthly blood loss during the years from menarche (start of first period) until menopause (complete cessation of menstruation).
There is no definitive medical explanation for RLS, and understanding an individual’s presentation is achieved by categorisation: into primary (or idiopathic) RLS or secondary RLS. Idiopathic RLS accounts for the vast majority of cases, and has no discernible root cause, except for a hereditary predisposition. This is according to the medicalised model however, and not a more holistic view point which we’ll also look at. Secondary RLS, as the name suggests, presents itself as secondary to other conditions such as liver disease, iron deficiency or pregnancy or iatrogenic (drug induced).
How does restless legs present itself?
RLS is classified as a neurological sensorimotor disorder. Sounds a convoluted description but that just means it’s of, relating to, or functioning in both sensory and motor aspects of bodily activity. That is, the pathways of the nerves that carry input and sensations to the central nervous system and initiate muscle response in the motor aspect.
functioning in both sensory and motor aspects of bodily activity. That is, the pathways of the nerves that carry input and sensations to the central nervous system and initiate muscle response in the motor aspect.
The disease carries significant increased risk for depression and anxiety disorders. While not life threatening, severe cases can disrupt sleep (causing insomnia), and potentially trigger anxiety and depression. Additionally, the pharmaceutical medication often given for restless legs can in fact, induce anxious or depressive states.
This common and debilitating nervous system condition is characterised by an “overwhelming and irresistible urge to move the legs”. Strange and unpleasant sensations in the legs and feet, often described as itchy or painful, cause an imperative to move as the issue can sometimes be temporarily ameliorated by doing so.
Typically, symptoms of restless leg syndrome is worse in the evening and at night, but can be experienced at any time of rest, depending on the severity of each individual’s experience. In many cases, RLS is considered to be a chronic and worsening condition, the impact that a disturbance of this magnitude has for one’s health, general well being and quality of life is significant.
Dopamine and the nervous system
 The neurotransmitter Dopamine has been found to play a role in many cases of RLS, as it is involved in controlling muscle movement. Dopamine is a neurotransmitter that plays a role in pleasure, motivation, and learning. It also acts as a messenger between the brain and nervous system to help the brain regulate and coordinate movement.
The neurotransmitter Dopamine has been found to play a role in many cases of RLS, as it is involved in controlling muscle movement. Dopamine is a neurotransmitter that plays a role in pleasure, motivation, and learning. It also acts as a messenger between the brain and nervous system to help the brain regulate and coordinate movement.
A dysregulated nervous system can wreak havoc on normal bodily functions. Supporting and nourishing our nervous systems is always of benefit, but especially when dealing with a condition such as RLS. Comorbidities (we hate this word, it sounds so depressing! But it means two or more conditions existing at the same time!) of anxiety and depression often occur alongside RLS. Whilst they are sometimes preexisting, they also arise as a result of living with a condition that disrupts one’s ability to rest.
Ensuring one has emotional support and talking therapies available to them when living with the symptoms of restless leg syndrome can offer much needed comfort. Stress is noted as being significantly higher in people suffering from RLS, as well as chronic stress being shown to lower dopamine levels. Taking steps to address stress is no mean feat, again, turning to others for encouragement and assistance is often necessary.
What factors influence restless legs?
Bearing all of the above in mind, in herbalism, we consider the nervous system, digestion circulation, excretory systems. There are generalised factors that can influence the symptoms of restless leg syndrome.
Questions we ask include:
Are the nerves well nourished? Consider herbs like vervain, oats, passiflora to calm and soothe the nerves.
Is there a balance between stress and relaxation?
Does a person do any exercise? (This has shown to help a lot with the severity of the symptoms).
What factors can influence the dopamine levels?
How is the overall nutrition and then how are the nutrients being absorbed?
Is the digestive function faring well? A healthy balanced diet can still provide inadequate nutrition if there is inflammation in the gut or irritable bowel type symptoms. We’d want to look at circulation and lymph drainage, again improved by massage and exercise.
Are the minerals sufficient? Epsom salt baths that promote magnesium have shown to reduce the muscular spasm associated with restless legs.
Is the circulation proficient, and is nourished blood getting to the legs? Ginger can help here but also regular exercise. Exercise helps reduce symptoms of restless legs syndrome, except late at night when it can often over stimulate and make the restless legs worsen.
Other beneficial solutions for symptoms of Restless Leg Syndrome
Yoga has been shown to be an incredibly beneficial practice for people suffering from RLS. Its positive effect on stress is widely acknowledged, as well as having a pivotal role in dopamine creation.  is another practice that has been shown to increase dopamine. Whilst its ethos centres rest as a powerfully transformative reclamation of one of our fundamental rights; something that RLS takes from so many.
is another practice that has been shown to increase dopamine. Whilst its ethos centres rest as a powerfully transformative reclamation of one of our fundamental rights; something that RLS takes from so many.
‘Good sleep hygiene’ is a term used to describe healthy habits focused around this essential aspect of life. Creating ritual and routine around significant aspects of our daily living is something humans have always done, from prayers of gratitude before meals to creating special ambiance for intimacy. Certainly, for children, there is often great care taken in orchestrating beneficial bedtime routines. But for many of us as adults, we disregard our need to honour the liminal space between day and night, activity and rest, of being awake and then asleep. Consider that valerian may be helpful here as long as the blood pressure isn’t too low as valerian is a wonderful muscle relaxant to help soften and improve the situation.
Some essential aspects of good sleep hygiene are listed below:
- Reducing or ideally eliminating caffeine, nicotine and alcohol before bed. (Each of these substances are stimulants and as such trigger our sympathetic nervous system (fight or flight), despite beliefs to the contrary about their place in relaxation)
- Endeavouring to keep to a regular sleep/wake schedule. (Allowing yourself to align as much as possible with the sun rise and set is a really powerful way to work with your circadian rhythm)
- Reducing exposure to light, specifically blue light emitted from screens prior to bedtime.
- Ensuring the bed space is a peaceful and relaxing environment.
Useful supplements for RLS
Anecdotal advice in conditions like RLS, where research studies are limited, can be fascinating and transformative for many people. Magnesium supplementation is often recommended for sufferers of RLS, particularly where it is lacking in their diet.
Magnesium supplementation is often recommended for sufferers of RLS, particularly where it is lacking in their diet.
Magnesium is a mineral that our bodies use for a variety of processes, including nerve and muscle function and regulation of the normal function of the central nervous system. Food sources of magnesium are green leafy vegetables, legumes, nuts, seeds, and whole grains.
Zinc is another mineral that some people find to make a difference to their experience of RLS. Zinc is an essential nutrient. Its role in supporting the body is vast, and it is present in many types of food from both plant and animal sources.
Another supplement often suggested for the symptoms of restless leg syndrome is vitamin D. Research has shown both the relationship to dopamine creation and the subsequent improvement in many cases of RLS.
Helpful herbs for RLS
When treating RLS with herbal preparations, it is important to do a holistic evaluation of yourself/your client, considering individual energetics (of person and plants) alongside history, lifestyle, symptoms and comorbidities (there’s that word again!).
There is a wealth of opportunity to positively affect our health and wellbeing when we turn to our herbal allies for support. Below are some suggestions for herbs to consider when addressing RLS.
Nervine herbs can be wonderful support for restless legs. The word ‘nervine’ is a herbal action that pertains to the plant’s ability to affect change on the nerves. Nervine herbs can be restorative and nourishing, stimulating or relaxing.
Nervine tonics – herbs that restore and nourish the nerves such as oat straw or milky oat seed. Oats can be taken as a tincture, but oats can be really beneficial for the nerves when eaten daily as porridge.
Nervine relaxants – herbs to gently relax the nerves allowing them to recover and restore.
Valerian (Valeriana officinalis)
Valerian is a nervine relaxant and restorative, known for sedative qualities. It’s of great value in treating anxiety and use in sleep disorder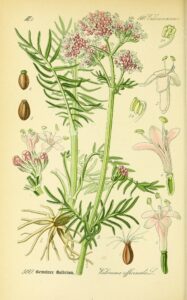 formulations. However, careful consideration of the individual’s constitution and energetics is necessary at all times.
formulations. However, careful consideration of the individual’s constitution and energetics is necessary at all times.
We love the musky smell of valerian, a wonderful central nervous system relaxant. We take a teaspoon of valerian decocted or simmered in a little water for 10 minutes, strained and added to milk and warmed through. With a teaspoon of honey this makes a delicious nighttime drink. We use fresh valerian root dug from the garden and the wiggly roots rinsed off, but dried valerian works well too.
Passion Flower (Passifloraceae)
One of our favourites! A slightly odd flavour, but oh so gently relaxing and soothing. This herb was used to create a truth serum from one of the compounds, Harmine, in WorldWar II Germany. It calms you to a blissful state of relaxation and euphoria, so much so that you might just answer any questions fired at you!
St John’s Wort (Hypericum perforatum)
St John’s Wort is a nerve restorative, fairly well known for use in depression and anxiety, and these particular indications are of immense importance when treating RLS. St John’s Wort has also been found to have an influence on dopamine levels which is another reason to consider this remedy for RLS.
Milk Thistle (Silybum marianum)
Milk Thistle supports the liver in the detoxification process. This medicine is particularly worth considering where RLS is worsened or triggered by consuming alcohol.
Nettle (Urtica dioica)
Nettle is abundant in minerals and particularly in iron. Anyone’s diet is greatly improved by including this powerhouse. RLS often occurs with reduced iron levels, and Nettle is an accessible and affordable way to up iron intake.
Herb-wise, we always look at the individual. How is the general state of the nervous system? Does it seem overexcited? Are there lots of daily stresses? Does there appear to be adrenal exhaustion? Whatever is going at a deeper level though, twitching legs indicates an inability for the nerves to completely rest and restore.